How on earth are we regulating human genetic modification?
author: Kevin Curran PhD
updated: 2-24-2024
We are now living in a world where a modestly funded lab with modestly trained technicians can use CRISPR to alter the human genome. That fact is both exhilarating and terrifying.
The possibility for greatness is intoxicating. DNA editing should allow scientists to correct mutations that lead to genetic disorders.
Diseases will be eradicated.
What’s not to like??
As one would imagine . . . there’s a flip-side to this scenario.
Mishaps may occur. Let’s be honest, mishaps will certainly occur.
New versions of genes will be introduced into babies without sufficient laboratory testing. In an attempt to create children with enhanced genetics, unregulated labs may accidentally produce horrific mutant babies whom bear the mark of painful developmental mutations.
The road to scientific progress is often bumpy, but it needn’t be strewn with casualties. The proper degree of regulatory oversight should allow genome editing science to mature in a safe and ethical manner.
Unfortunately, we’ve already seen what happens when medical science races forward in the absence of proper oversight.
In Novemeber 2018, a Chinese scientist named He Jiankui created the world’s first genetically edited babies. He used CRISPR technology to introduce mutations into a gene called CCR5. In theory, if the CCR5 gene is mutated to the point of being non-functional, then the HIV virus will be incapable of entering and destroying Helper T cells. If all goes perfectly, then He will have created children that are immune to AIDS. The problem is, He went about this process with very little regard for the twin girls in the experiment. He moved forward with the procedure after he learned that his mutations had never been tested in animals. Animal testing in mice would at least determine whether this new CCR5 gene creates a toxic protein.
He Jiankui’s approach to this project has led to widespread criticism from scientists, ethicists and government officials.
Once the details of He’s work were revealed, it became clear that although human embryo editing is relatively easy to achieve, it is difficult to do well and with responsibility for lifelong health outcomes. ~Jennifer Doudna
A Shenzhen court found He Jiankui guilty of ‘forging ethical review documents and misleading doctors into unknowingly implanting gene-edited embryos into two women.’
In 2019, He was sentenced to three years in Chinese prison for ‘illegal medical practices’. It remains unclear what has became of the twin CRISPR babies, Lulu and Nana. He has stated that they are living private lives as normal and healthy children.
2024 update:
In February of 2023, He began speaking to the press again, he acknowledged that he ‘moved too quickly‘ with his human editing experiments.
In June of 2023, He revealed he is once again embarking on new ventures to modify human embryos via gene editing. These new pursuits will target Duchene Muscular Dystrophy as well as age related disease, such as Alzheimer’s disease. According to He, funding has already been secured through private and anonymous investors.
In a succinct, one page document, He proposed research that would involve gene-editing mouse embryos and then human fertilized egg cells, or zygotes, in order to test whether a mutation “confers protection against Alzheimer’s disease.”
Source: CNN
He Juankei is a man on a mission… and he is clearly undeterred by past missteps. I think his actions underline the limited capacity that institutions hold in terms of preventing new technology from being deployed.
What have we learned here?
If nothing else, the CRISPR baby story illustrates that a single headstrong individual can begin genetically modifying humans with very little oversight.
This begs the question…. who is regulating the future of genetic modification?
Is CRISPR legal in the US?
Below, I will assess CRISPR regulations on both a national and global level.
First, let’s clarify why we need regulation in this arena.
Kevin Curran PhD is the founder of Rising Tide Biology
Hit the subscribe button below to follow Kevin’s newsletter on Substack.
In 2024, I am focused on a DIY approach towards designing new medicine. I’m using an AI software platform to develop a new drug and I will be sharing all insights with my audience. Join the adventure!
Why do we need to regulate human germline editing?
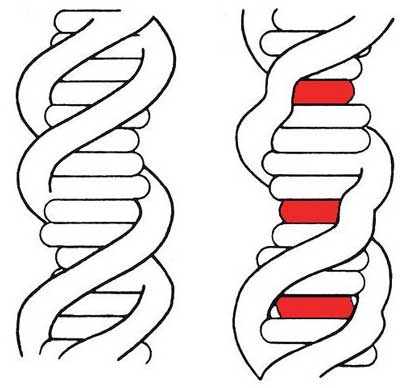
Germline edits are directed at genes held within sperm cells, eggs or embryos. DNA edits produced in these germ cells are passed on to children and, in doing so, may alter the downstream human lineage.
In contrast, DNA edits delivered to non-germline cells, like adult skin cells, are called somatic cell editing. Somatic cell edits will only alter the treated individual and are much less controversial than germline editing. I provide more detail on this distinction in a video at the bottom of this article.
I think the science community should move forward with CRISPR in both the context of somatic cell and germline cell edits. In the U.S., the FDA already endorses clinical trials for CRISPR editing in adult, somatic cells (immune cells, bone marrow stem cells). Once, we can perform these edits safely and accurately, we should move on to editing germline cells. We should move in this direction because genome editing technology can alleviate human suffering by reducing the incidence of genetic disorders.
That said, we need to be methodical and cautious. Genome editing brings hope but also inherent risks. These risks should be taken seriously.
Below, I briefly list my main concerns with human germline edits.
- Toxic proteins: Germline edits may produce toxic proteins. Before moving forward with a specific protocol in humans, we must ensure any altered gene has been tested for safety in cell culture and animals.
- Off-target edits: Genome editing technology, such as CRISPR, can accidentally deliver genetic changes to unintended regions of our genome. These are called off-target edits and we want to eliminate, or massively reduce, the chance of off target edits before moving forward with germline edits.
- Mosaicism: Mosaic embryos are another concern. When a genetic alteration is applied to germ cells, we commonly find that the alteration does not reach all the cells in the developing embryo. Some cells receive the edit, while other remain unedited, hence the term mosaicism. It’s not possible to predict the outcome of an unevenly altered embryo.
- Lifestyle edits: At it’s best, scientific innovation offers the chance to reduce human suffering. Human genome edits that eradicate a painful genetic disorder are certainly worth pursuing. In contrast, human genome edits that aim to enhance human life (i.e. taller and smarter babies) do not offer a reduction in suffering and, thereby, are not necessary.
- Heredity: The primary reason germline edits require careful regulation is because this treatment can alter the human lineage. We are all part of the human species and the decision to alter our genetic code shouldn’t lie solely in the hands of rogue scientists. While government bureaucracy and a committee mentality can often stifle innovation, I do think institutional oversight will be a necessary component to guide any heritable alterations.
US laws on human genetic engineering
Each nation has the option of setting their own rules and guidelines on genetic modification of humans. Below I will review the regulations here in the US.
US regulations on gene therapy
First and foremost, there is no federal legislation that bans protocols or places restrictions on experiments that manipulate human DNA.
CRISPR is legal in the US. Many hospitals and biotech companies are currently pursuing clinical trials with CRISPR. These trials are regulated by the FDA. If the trials are successful then the FDA will grant these organizations approval to market the drug as a commercial product. The US government supports the exploration of CRISPR in the context of these regulated clinical trials. Companies such as Intellia, Editas and CRISPR Therapeutics are pushing this technology forward. I suspect we will see a CRISPR based drug reach the market in 2-3 years (2023-2024).
Below, I summarize the key provisions of federal control of CRISPR experiments.
Federal control exists in terms of:
1.) Allocating federal funding towards genome edit research projects. In 1995, the Dickey-Wicker Amendment passed, which forbids the NIH from funding research involved in the manipulation of human embryos.
2.) Approval to run gene therapy clinical trials on humans. In 2015, Congress passed a provision stating that the FDA must approve any human clinical trial that involves gene editing. The FDA will certainly reject human trials that modify the human lineage via germline edits.
3.) Awarding FDA approval in terms of a marketable product. If you want to sell your DNA treatment in the US, you need FDA approval before marketing your procedure as a cure, treatment or prevention against a disease. The FDA will not allow a human germline alteration to enter the marketplace.
There is a bit of a loophole in these provisions. If you don’t rely on federal money, you aren’t testing your CRISPR process on humans and you don’t intend to sell on the U.S. market, then you are free to pursue genome editing. For example, there is no law against ordering CRISPR tools off the internet and using them in your garage to experiment on bacteria.
As of 2023, the official position of the FDA is:
- federal money can be used to research somatic cell gene therapy
- federal money cannot be used to research germline cell gene therapy
Here is the relevant quote from the FDA site.
Current gene therapy research has focused on treating individuals by targeting the therapy to body cells such as bone marrow or blood cells. This type of gene therapy cannot be passed to a person’s children. Gene therapy could be targeted to egg and sperm cells (germ cells), however, which would allow the inserted gene to be passed to future generations. This approach is known as germline gene therapy.
The idea of germline gene therapy is controversial. While it could spare future generations in a family from having a particular genetic disorder, it might affect the development of a fetus in unexpected ways or have long-term side effects that are not yet known. Because people who would be affected by germline gene therapy are not yet born, they can’t choose whether to have the treatment. Because of these ethical concerns, the U.S. Government does not allow federal funds to be used for research on germline gene therapy in people.
For more information on the FDA’s position, you can dive into their 2022 guidance document on Human Gene Therapy.
Recent FDA approvals?
In theory, you could operate a privately funded lab and conduct non-clinical, human gene therapy research. However, if you ever wanted to sell your therapy in the US, you will need FDA approval for clinical studies and marketing. As of 2021, only somatic cell gene therapy products have been awarded approval in the US. There are no instances of a germline gene therapy product in the US.
Below I list the FDA approved gene therapy products. (updated 2023)
- Kymriah ~ a CAR-T therapy: T-cells genetically modified to kill lymphoma and leukemia cancer cells (Novartis)
- Yescarta ~ a CAR-T therapy: T-cells genetically modified to kill lymphoma cancer cells (Kite/Gilead)
- Breyanzi ~ a CAR-T therapy: T-cells genetically modified to kill lymphoma cancer cells (BMS)
- Luxturna ~ an AAV vector delivers RPE65 gene into the retina of patients with rare eye disease (Spark)
- Zolgensma ~an AAV9 gene therapy delivers SMN1 gene to the motor neurons of SMA patients (Novartis)
- Abecma ~ a CAR-T therapy: T-cells genetically modified to kill multiple myeloma cells (BMS)
- Carvykti ~ a CAR-T therapy: T-cells genetically modified to kill multiple myeloma cells (J&J/Legend)
- Hemgenix ~ an AAV gene therapy for patients with Hemophilia B (Factor IX deficiency) (CSL Behring)
- Skysona ~ Hematopoetic stem cell therapy to treat rare neurologic disease, CALD (BluebirdBio)
- Zynteglo ~ Hematopoetic stem cell therapy to treat b-thalassemia, CALD (BluebirdBio)
All of these approved gene therapy products affect only somatic, adult cells.
Luxturna affects retinal eye cells. Zolgensma alters motor neurons. The CAR-T drugs affect immune cells that circulate in our blood. None of these genetically altered cells will develop into sperm or egg cells.
None of these therapeutic genetic changes will be passed down to the children of treated patients.
FDA CRISPR regulations
In response to recent advances in the world of CRISPR and DIY gene therapy pursuits, the FDA attempted to clarify their stance with the following statement.
Nov. 2017: FDA considers any use of CRISPR/Cas9 gene editing in humans to be gene therapy. Gene therapy products are regulated by the FDA’s Center for Biologics Evaluation and Research (CBER). Clinical studies of gene therapy in humans require the submission of an investigational new drug application (IND) prior to their initiation in the United States, and marketing of a gene therapy product requires submission and approval of a biologics license application (BLA).
State Laws on CRISPR?
On July 30, 2019, the first American law was passed that regulates the use of CRISPR.
Republican state senator, Ling Ling Chang, wrote a bill for California state law that prevents companies from selling CRISPR kits designed to modify human DNA. This bill was obviously written as a direct challenge to Josiah Zayner, a California resident that operates a company called The Odin. This company sells genetic-engineering supplies. At one point, The Odin did offer a kit to modify a human gene called myostatin. However, that kit is no longer for sale. The company does still sell CRISPR kits that enable users to modify bacteria DNA.
Global regulations
There’s not much to talk about here… International regulations on genome editing are tenuous at best.
As of 2023, there are NO cohesive, legally binding or universally recognized set of rules in the international arena of gene therapy or genome editing.
The Declaration of Helsinki may be the closest document we have in terms of an international set of guidelines for human experimentation in medicine. The Declaration of Helsinki was formed in 1964, largely as a reaction to the horrific experiments carried out by Nazis in WW2. The document codifies various ethical standpoints on human experimentation. As a non-legally binding document, the Declaration of Helsinki only has power when it’s cited in national regulations. This declaration has undergone a series of revisions. The FDA in the US has rejected all revisions after 2000. In 2006, the FDA announced it will eliminate all reference to the Helsinki Declaration in their national regulations. The European Union still cites the 2000 revision.
In August 2019, the World Health Organization (WHO) announced their plans to establish a public registry to include both somatic (adult) and germline clinical trials. The WHO is clearly attempting to improve transparency in human DNA alterations. This registry may be the first step by the WHO to develop a global governance framework for human genome editing. If nothing else, their registry makes it easier to identify the rogue scientists. If you are conducting human genome editing but have not registered with the WHO, then presumably you are acting in bad faith or have something to hide. In theory, there could be career consequences with this misstep, however, at this time there are no direct penalties associated with leaving the WHO uninformed regarding your germline edit experiments.
An international group called HUGO also provides a legal baseline in terms of gene therapy actions, but it is not clear if this group has any global authority.
China genome editing regulations
After the CRISPR babies situation in China, the Chinese government has issued new regulations. These new regulations state that clinical gene editing research requires national approval.
…the Chinese government this week issued draft regulations that would require national approval for clinical research involving gene editing and other “high-risk biomedical technologies.
What’s the difference between somatic and germline gene therapy?
Somatic cells are adult human cells. These are cells from our body that have zero chance of developing into eggs or sperm cells. DNA modifications made to somatic cells will not carry over to the children of the treated patient.
Most people are comfortable with the idea of somatic cell modifications. For the most part, the US government is comfortable with experimental therapies that explore genetic changes in somatic cells (i.e. CAR-T cell therapies). In fact, the FDA has already approved cancer therapies that involve creating genetic changes to T cells in our immune system (Yescarta, Kymriah, etc.)
In contrast, germline cells include sperm, eggs or embryo cells.
DNA modifications delivered to germline cells may be carried into the next generation of humans. In theory, a germline DNA modification could eventually alter the human lineage. The genetic change will carry into your children and your children’s children and so on and so forth…
Most people are very uncomfortable with germline genome modifications. As you may have expected, the federal government does not condone genetic modification of sperm, eggs or human embryos.
Here I am explaining somatic vs. germline genome edits to a biotech audience.
Kevin Curran PhD is the founder of Rising Tide Biology
Hit the subscribe button below to follow Kevin’s newsletter on Substack.
In 2024, I am focused on a DIY approach towards designing new medicine. I’m using an AI software platform to develop a new drug and I will be sharing all insights with my audience. Join the adventure!